New NUH procedure reduces side effects for prostate cancer patients undergoing radiation treatment
A rectal spacer acts as a physical barrier to increase the distance between the prostate and the rectum, in order to protect the rectum from unwanted exposure to radiation.


This audio is generated by an AI tool.
SINGAPORE: Prostate cancer patients undergoing radiation treatment can now experience fewer side effects such as bleeding, with the introduction of an innovative procedure that minimises radiation exposure to the rectum.
This new rectal spacer technique has been used by doctors at the National University Hospital (NUH) to enhance treatment outcomes and improve the quality of life for such patients.
A rectal spacer acts as a physical barrier to increase the distance between the prostate and the rectum, in order to protect the rectum from unwanted exposure to radiation.
This intervention reduces the likelihood of long-term, debilitating side effects that can lead to frequent hospitalisation.
PROTECTIVE BARRIER AGAINST RADIATION EXPOSURE
Prostate cancer is the most common cancer affecting men in Singapore, and usually occurs in men over the age of 50.
According to the Singapore Cancer Registry Annual Report 2021, it made up nearly 17 per cent of cancer diagnoses among males, with 6,912 cases reported from 2017 to 2021.
Since May 2022, 150 patients have benefitted from the minimally invasive outpatient procedure, said the National University Health System (NUHS) in a press release on Monday (May 20).
The 15-minute procedure, performed under general anaesthesia, involves the implantation of a gel-like substance that acts as a barrier between the prostate and rectum during radiation treatment.
It has shown promise with no major adverse reactions among the treated patients, NUHS added.
For patients undergoing external beam radiation therapy, the rectal spacer technique reduces the risk of radiation-induced damage leading to complications like rectal bleeding.
Such therapy involves beams of radiation from a machine being focused on a patient’s prostate. Patients undergo treatment five days a week, for about four to eight weeks.
“Reducing the risk of radiation-induced side effects is a priority for us, as up to 10 per cent of patients may experience clinically significant side effects that last beyond three months following the completion of radiation therapy,” said Adjunct Associate Professor Jeremy Tey, senior consultant in the Department of Radiation Oncology at the National University Cancer Institute, Singapore (NCIS).
“A small proportion of patients may have rectal bleeding so severe that they require blood transfusions at the hospital. It’s important that we continuously look at ways to improve patient outcomes and quality of life,” he added.
REDUCING DAMAGE TO NORMAL TISSUES
The challenge with radiation therapy for prostate cancer patients involves targeting the cancer effectively while minimising damage to surrounding tissues, said doctors.
“Radiation is one of the very established treatments now for prostate cancer, and part of the radiation involves targeting the prostate. Despite advances in radiation, we can't make that radiation zone perfect, and the rectum sits just behind the prostate,” said Dr Arshvin Kesavan, associate consultant at the NUH’s Department of Urology.
“The way radiation works is … it causes cancer cell death. But of course, it's not so discriminatory and it can harm normal tissue as well. If that tissue is in that radiation zone, it can get affected.”
NUH urologists use biodegradable rectal spacers that are absorbed by a patient’s body after a period of time. These are approved by the United States Food and Drug Administration and Singapore’s Health Sciences Authority.
The procedure is tailored to each patient’s specific situation. It also takes into account the size, location and invasiveness of the tumour, as well as individual anatomical factors.
The technique has changed the way that prostate cancer patients are now looking at radiation, Dr Arshvin told CNA’s Singapore Tonight on Monday.
“Before this, they'd be very concerned about these types of side effects. But now that they know we have this protection, radiation is becoming a lot more accessible to people and more acceptable to people.”
ENHANCING QUALITY OF LIFE FOR PATIENTS
When the rectum is exposed to radiation without a protective gel in place, about 20 to 30 per cent of patients could suffer from side effects, noted Dr Arshvin.
“That could be as mild as maybe going to the toilet more frequently. But it can be as severe as developing ulcers which bleed, and when this problem happens, there's no good treatment,” he added.
“So it can be a recurring issue even years after radiation has been completed.”
Out of the 150 patients who benefitted from the procedure, none had serious rectal ulcers. The number of patients who experienced minor symptoms after the gel was in place also dropped, from 30 per cent to 4 per cent, Dr Arshvin said.
Patients with locally advanced prostate cancer such as cancer that has invaded the wall of the rectum; those with pre-existing urinary retention; and others at high risk under general anaesthesia may not be offered the procedure.
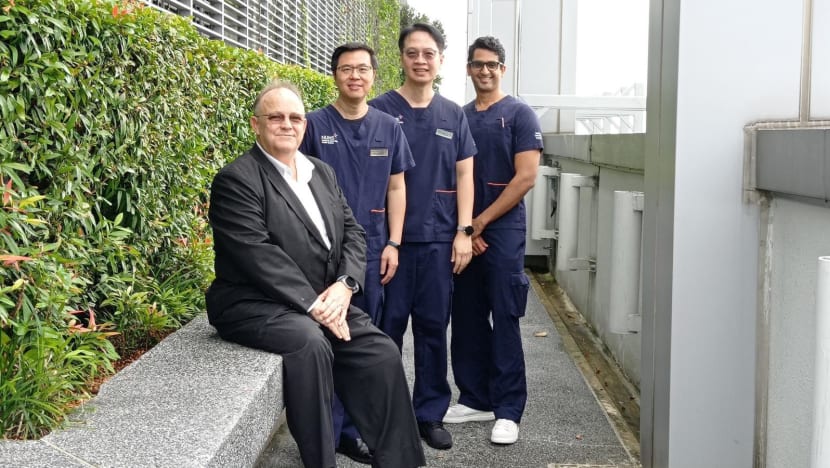
Among those who have gone through the procedure is Mr David Peter Dowdell, who was diagnosed with prostate cancer last year.
The 63-year-old did not hesitate when offered the option, and went for it last September.
Nearly a month later, the director in a technology firm started his radiation therapy and has had 41 such sessions at the NCIS over two months.
“Medically sometimes, you can't have this gel,” said Mr Dowdell, who experienced no side effects from his radiation.
“But for those who can, it shouldn't be an option. It should be part of the process.”
The NUH team is providing training of this new procedure to surgeons at other public hospitals.
Associate Professor Edmund Chiong, head and senior consultant at NUH’s Department of Urology, said: “By adopting this technique, we are not just aiming to treat prostate cancer.
“We are also focused on enhancing the comfort and improving the quality of life for our patients during and after treatment.”
















