Invisible, incurable, constantly in pain: This is what living with fibromyalgia is like
Imagine doctors insisting that you are fine, when your body is engulfed in pain. Four fibromyalgia patients tell CNA Insider about their struggles with this invisible illness and how they draw strength from their suffering.
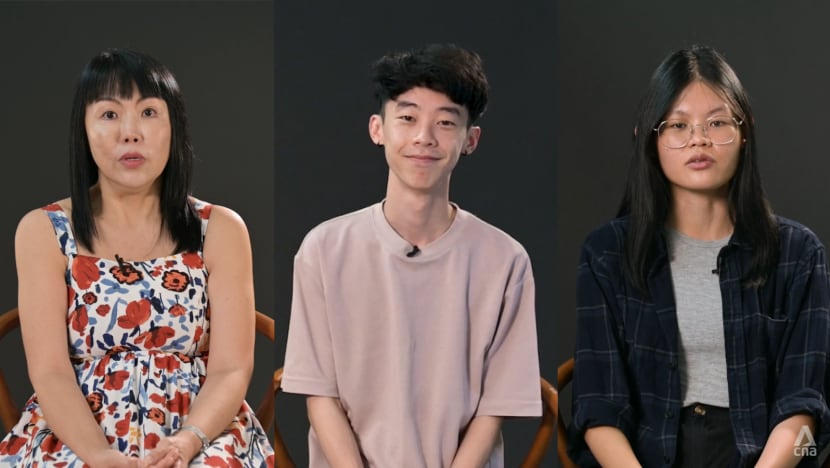
(From left to right): Daisy Chia, Ong Jin Jie and Rina Ong sat down with CNA Insider to share their struggles with fibromyalgia.

This audio is generated by an AI tool.
SINGAPORE: At first glance, Ong Jin Jie is an upbeat 29-year-old multi-hyphenate. He is co-founder of a media agency, an adjunct lecturer at two polytechnics, a property consultant, a podcast host and a songwriter.
Few would suspect that he is also a victim of chronic pain.
His symptoms started in 2019 with mild body aches, fatigue and fever, which later escalated into an intense, to-the-bone pain that sent him looking for answers.
He pored over academic papers on autoimmune diseases and invisible illnesses, experimented with acupuncture, cupping, herbal remedies and other alternative treatments, and even sought spiritual healing from churches and temples. But nothing hit the mark.

Western medicine provided no more clarity for Rina Ong when she started experiencing similar pains. “It felt like someone … stabbing my knee,” described the 31-year-old, who also broke out in hives all over her body.
She sought medical advice, but 18 negative blood tests and one clean nerve examination later, her doctors insisted that she was in the pink.
“Maybe it’s in your mind,” several doctors even suggested to Daisy Chia, who grappled with brain fog, mood swings, lethargy and incontinence in addition to chronic pain.
“(One doctor) sent me back with nothing, not even painkillers,” recounted the 54-year-old, who kept wondering, “Am I getting crazy?”
“Clara”, 25, who declined to be identified, knew for a fact that the only thing she was “faking” was the amount of pain she chose to tell others she was suffering.
Such is the nature of fibromyalgia: invisible to the eye, undetectable by tests and confounding to medical professionals, yet painfully real for those who endure it.
Four individuals opened up to CNA Insider about what living with fibromyalgia is like and how they came to terms with their chronic condition.
WATCH: Living with chronic pain that even doctors don’t believe — This is fibromyalgia (12:39)
WHY DIAGNOSIS IS DIFFICULT
Given that fibromyalgia, or fibro for short, does not result in any observable bodily damage, not only is it invisible, but also there is currently no medical test that can confirm its existence.
“Most doctors would recognise the term ‘fibromyalgia’ and that it’s a medical condition,” said Singapore General Hospital consultant Adeline Leong, a pain medicine doctor.
However, they may not understand it very well … purely (because) it’s something that isn’t that common.”
Nearly one in 20 people globally are estimated to have fibromyalgia. Compared to men, nearly twice as many women, or more, are affected. In Asia, the neurosensory disorder is not studied relatively much, and even lower incidence rates are reported.
What is clear is that the term “fibromyalgia” has come to describe a chronic musculoskeletal pain that is often accompanied by fatigue, cognitive and sleep disturbances and other psychiatric and somatic symptoms.
But diagnosis of fibromyalgia remains difficult. For instance, during her initial visits to accident and emergency, Rina’s doctors speculated that she had a rheumatic condition because of her acute joint pains.
Hypothyroidism is another common misdiagnosis due to overlapping symptoms, like low vitamin D and calcium levels.
An actual fibro diagnosis is associated with pain experienced throughout the body for more than three months, based on the Widespread Pain Index (WPI), a self-assessment that measures the distribution of pain across the body and rates the severity of symptoms.
Even then, the WPI is not regarded as hard evidence by medical standards.
Pain perception is subjective and dependent on individual tolerance levels. Factors such as stress, sleep quality, mental state, pain management strategies and personal pain experiences could also impact an individual’s WPI, said Leong.

Furthermore, no two fibro patients are the same.
Clara likened her pain to “a rubber band around your hand” — a numbness crawling from her neck, down her spine and into her limbs. Daisy, meanwhile, struggles with brain fog to the extent that she sometimes cannot recognise the way home.
Likewise, Jin Jie and Rina endure different forms of pains: a deep-seated ache for Jin Jie and a stabbing sensation for Rina.
Such a mixed bag of symptoms makes it difficult for the medical community to interpret a fibro patient’s distress, let alone prescribe suitable treatment.
‘MY LIFE IS OVER’
The absence of a cure brings another form of anguish besides chronic pain.
Upon receiving their diagnosis, the weight of their condition sank in faster than Clara and Rina’s relief at having their pain acknowledged.
“It could’ve been something so serious, like cancer, and I honestly think I’d have felt happier,” said Clara, diagnosed in 2020. She was angry that it was not a curable condition or at least one that was more familiar to people.

All that Rina could remember was standing outside the clinic and doubling over as she cried and thought, “My life is over.”
Jin Jie more readily accepted his condition but could not help wondering why this was happening to him. “Where did I go wrong?” he questioned.
Experts hypothesise that fibromyalgia stems from dysregulation of the body’s central nervous system, whereby patients experience significantly more pain than others, despite sustaining similar injuries.
Other studies have also noted that fibro patients often share a history of verbal, physical and/or sexual abuse.
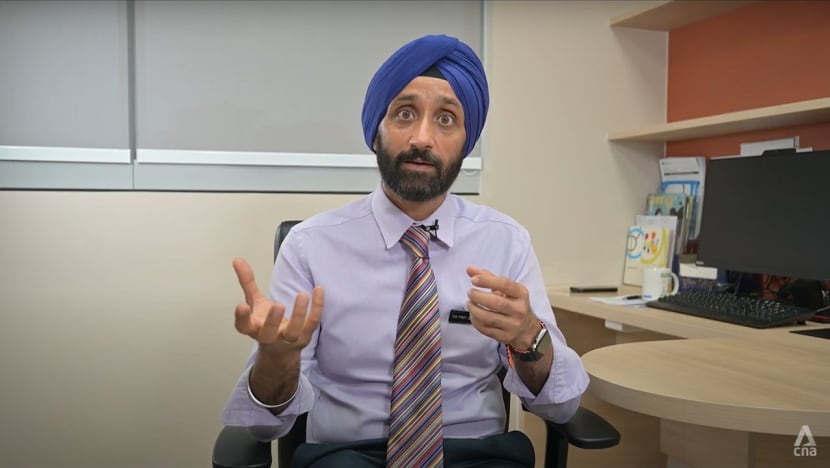
After all, chronic pain not only is about what’s wrong in the body, but also involves pertinent social and psychological factors, said Prit Anand Singh, the director of Changi General Hospital’s chronic pain management service.
Similarly, traditional Chinese medicine (TCM) suggests that encounters with unhappiness or distress can trigger fibromyalgia. TCM attributes this to “the liver’s vital energy”, which is believed to be linked to mood regulation.
When a person maintains a relaxed and cheerful emotional state, said physician Ng Hern with the Singapore Chinese Physicians’ Association, the liver’s vital energy naturally balances, potentially reducing pain symptoms.
For Rina, learning about the traumatic connections between her past and her present condition marked a turning point. She had sought psychiatric help, and her psychiatrist traced her trauma back to her parents’ separation.
She then understood that she had never fully processed those emotions. She recounted her doctor saying: “Don’t you think that, actually, your body’s telling you to take care of yourself better now?”
These words struck a chord, changing her perception of chronic pain as a burden to an opportunity to embrace and nurture herself.

FINDING STRENGTH, AND THE RIGHT PEOPLE
While Rina had accepted her chronic condition, she held out little hope that potential partners would take on the lifelong responsibility of caring for her.
In fact, she disclosed her condition to a date during their first meeting, fully prepared for him to decline further contact.
But her uncertainty lifted when he said she was beautiful, inside and outside, and had braved so much in life. They are now married.
Concern over the material and emotional strains placed on loved ones is common to many who have a lifelong disorder. Daisy, for example, worried for years that she had not been a very present mother to her three children.
When she expressed her regrets to her eldest son, he hugged her tightly, she recounted. And he assured her: “All my great memories of my childhood are always with you.”

What Rina has come to realise is that “there are people (who) will see you beyond your illnesses and see your pain as your strength”. She added: “You just need to find the right people.”
There is always an underlying fear, however, that “the right people” are few and far between, especially in the workplace.
Clara, a civil servant, said: “I fear that (my bosses) would choose not to promote me … that they’d consider my peers over me, just because I have a condition like fibro.”
To conceal her condition, she often slips into the toilet to take painkillers — which provide limited relief — before returning to her desk.
Fibro patients are not unique, however, in regard to productivity loss. In 2018 alone, episodic migraines were said to cost Singapore about S$1 billion, largely due to missed workdays and reduced output.
And in 2016, according to research published last month and funded by the Ministry of Health and Temasek Foundation Innovates, productivity loss associated with adverse childhood experiences (including child maltreatment, dysfunctional home environments and bullying) was estimated at S$489 million.
To manage stress and thus their symptoms, fibro patients are advised to make holistic lifestyle adjustments.
Clara has found that incorporating more greens into her diet and maintaining a regular exercise routine can help to regulate pain flare-ups, while Jin Jie relies on weekly psychotherapy sessions and practises emotional mindfulness.
There is no one-size-fits-all approach to managing fibro symptoms, but one universal strategy — for anyone with chronic pain — involves finding a supportive community.
To this end, Rina and Daisy have set up support groups for fellow chronic pain sufferers on Instagram and Facebook, where they feature community members, organise meet-ups and share encouraging posts.
Jin Jie is also active on Instagram, sharing glimpses of his everyday life with fibromyalgia and helping others with similar struggles to feel less isolated.
And as they now share their stories, Clara hopes this will bring visibility to an otherwise invisible illness. “Fibromyalgia is a very real condition,” she said. “There are people who are suffering, even though they don’t look like they’re suffering.”